Confronting a Triple Threat: Diabetes, Kidney Disease and High Blood Pressure
According to the Centers for Disease Control and Prevention, more than 38 million people in the United States have diabetes, which is about 10% of the population. Most cases are Type 2, which usually happens in adults and means the body can't use insulin properly, causing blood sugar to go up and leading to various health issues.
“It is very common for individuals with diabetes to develop high blood pressure,” says Amy Michael, MS, RDN, LDN, CDCES, a registered dietitian nutritionist and certified diabetes care and education specialist who supervises the diabetes program at Carroll Hospital, a Lifebridge health center in Westminster, Maryland. “Many of the individuals we see also have declining renal function, as evidenced by their bloodwork.”
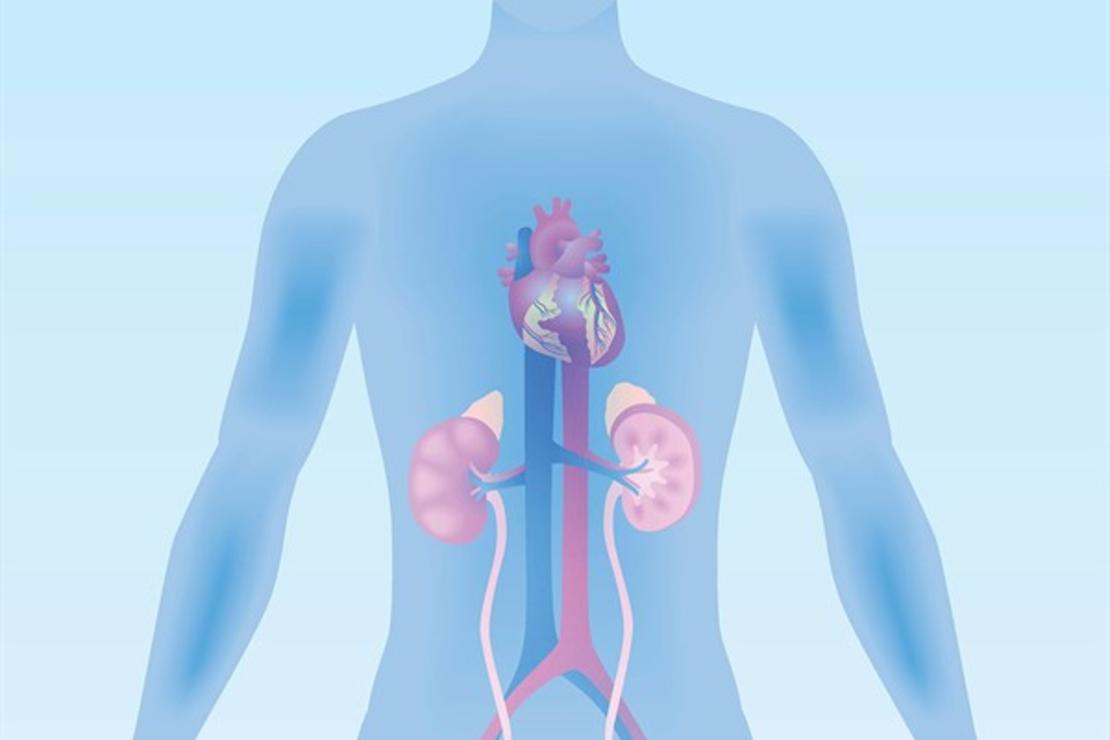
According to Michael, the kidneys filter waste in the blood to help remove it from the body. “Having increased glucose levels in the blood and/or high blood pressure damages blood vessels in the kidneys. This damage prevents our kidneys from filtering or removing the waste from our blood. This kidney damage may progress, and individuals may require dialysis to filter the blood.”
Michael says many studies indicate that, if left uncontrolled, diabetes and high blood pressure can increase the risk of chronic kidney disease. According to the CDC, an estimated 1 in 3 U.S. adults with diagnosed diabetes also have chronic kidney disease. The National Kidney Foundation estimates up to 40% of people with Type 2 diabetes eventually will develop kidney failure.
A Silent, Complex Relationship
This triple health threat confronts tens of millions of people in the U.S. but often goes overlooked until it becomes unavoidable. “Unfortunately, many people have one or more of these conditions without even realizing it,” Michael says. She notes that people can have elevated blood glucose levels or elevated blood pressure without experiencing any symptoms. And most people with kidney disease don’t have symptoms until they are in the later stages of the disease, which makes it harder to treat. “In general, I feel that many of us don’t see the doctor unless we have diagnosed conditions or are feeling poorly, which delays the diagnosis and treatment of diabetes and high blood pressure. If these conditions are not treated or controlled, they can increase the risk of kidney disease,” she says.
Additionally, the intricate relationship between diabetes, high blood pressure and kidney disease can be challenging for patients to comprehend. “I don’t think that most individuals understand the connection between diabetes, high blood pressure and kidney disease,” Michael says.
Fortunately, there are a few ways to treat, manage and prevent these conditions.
Promoting Heart and Kidney Health
“If you have a family history of heart disease and/or diabetes, the best thing you can do for yourself is get screened on a yearly basis,” says Michael. “Attend community blood pressure and diabetes screenings, make sure that you see your primary care provider yearly and have blood work done that can be used to diagnose diabetes and kidney disease.”
Michael says people with diabetes should know their ABCs:
- A: A1C under 7%
- B: Blood pressure under 130/80 mm/Hg
- C: Cholesterol — LDL (bad) cholesterol under 100 mg/dL; HDL (good) cholesterol over 40 mg/dL for men and over 50 for women; triglycerides under 150 mg/dL
“The cornerstone in the treatment for all three disease states” is lifestyle changes, she says. “Diet, physical activity, stress management and sleep behavior impact overall health. Weight loss can have positive impacts on health by helping to reduce both blood glucose and blood pressure values. Improved glucose and blood pressure control can help reduce the risk of kidney disease.”
According to Michael, simple first steps to eating better include:
- Increasing fresh or frozen fruits and vegetables
- Adding fiber into the diet by choosing whole-grain foods
- Consuming more water and limiting sodium intake
She also says increasing physical activity can help. “Both the American Diabetes Association and American Heart Association encourage most adults to aim for 150 minutes of moderate activity spread throughout the week. Remember, you can start with just 10-15 minutes/day and gradually build up to that goal!”
Medications That Can Help
Michael also says that adding in medications can help lower blood sugar while also protecting your heart and kidneys. Some of these prescription medications include:
- SGLT2 inhibitors. These oral medications help lower blood sugar and prevent kidney sugar reabsorption, benefiting kidney health. Some also help reduce the risk of heart attack, stroke and kidney disease progression.
- Finerenone. A non-steroidal mineralocorticoid antagonist (MRA), this oral medication benefits those with Type 2 diabetes-related kidney disease by preventing kidney fibrosis, potentially improving kidney and heart outcomes.
- GLP-1 RAs. These drugs can be taken orally, or they can be injected. They help stimulate insulin production and lower glucose and need to be taken with meals. Suitable for those on dialysis, these medications are recommended for individuals with kidney and coronary artery disease. They also address albuminuria and effectively reduce A1C levels, blood pressure, cardiovascular event risks and blood sugar.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs). Before newer drug options emerged, these medications were the two main options for protecting kidneys and managing blood pressure with Type 2 diabetes. Both oral medications have been used since the 1980s and are recommended for kidney disease, high blood pressure and other cardiovascular issues. They protect glomeruli, small filters in the kidneys that help in the filtration of blood. They also reduce albumin-creatinine levels, proteins associated with kidney damage, and lower cardiovascular disease risks. These medications effectively lower blood pressure, slow kidney and heart damage, and reduce the risk of heart attack or stroke. They benefit individuals with kidney disease or heart failure, even without high blood pressure, and are both considered equally effective.
While these drugs can have side effects or can be expensive, there are plenty of options to explore with your health care team. “I remind people that diabetes is a progressive disease that can be difficult to manage over time. The requirement of medication isn’t a bad thing or a sign of failure,” says Michael. “SGLT2 inhibitors and GLP-1 receptor agonists can be used initially for the diagnosis of diabetes or as an add-on therapy. Prescribing these drugs may be slow because these are the two newer drug classes in the treatment of diabetes and there are more medications being approved in these classes. Still, as the research continues to indicate efficacy for diabetes, heart disease and kidney disease, I think prescribing will increase.”
Seek Solutions to Challenges
Navigating the costs associated with treating and managing kidney disease, diabetes and high blood pressure can pose many challenges. However, assistance is available. Explore options such as discount cards for medication savings and consult your health care team to devise an affordable plan. Also, prescription assistance programs from drug companies and resources such as Social Security or co-pay assistance can help provide financial relief.
Juggling a varied health care team can also be tricky. Still, effective communication among doctors, especially when managing multiple health conditions, is key. Designating a primary physician advocate can help you ensure cohesive medical guidance from your whole team.
But Michael says, “The great news is that we now have more treatment options than ever before that target glucose control, help reduce death from cardiovascular disease as well as reduce deaths associated with kidney disease.”